
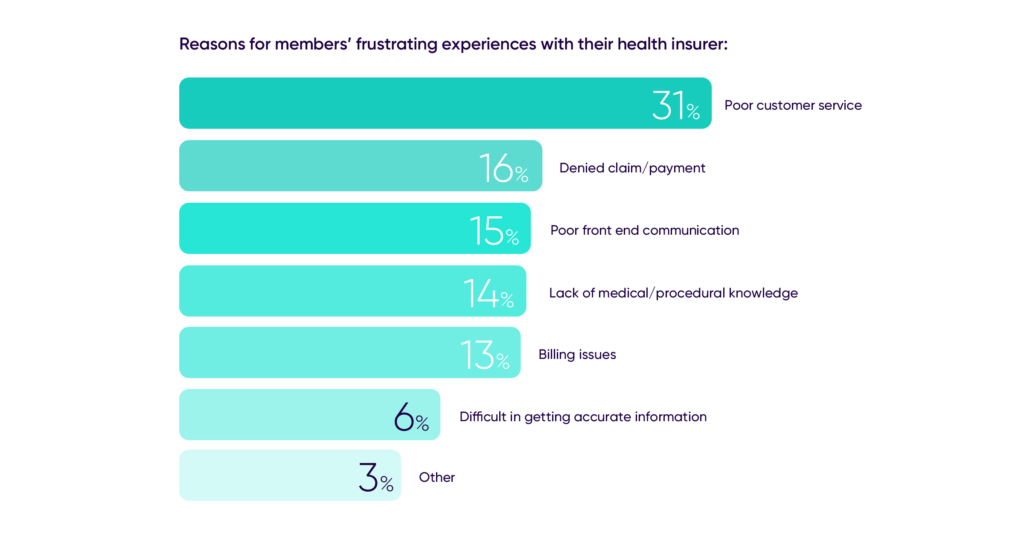
Healthcare insurers can improve the member journey and enhance the member experience by leveraging AI technology in their contact centers. The rising expectations of health insurance members for convenient and quality service necessitate a shift in the way insurers engage with their members. According to a Talkdesk Research™ report, 78% of health insurance members have experienced less-than-seamless experiences, with poor customer service, communication issues, difficulty in obtaining information, and long call wait times being cited as sources of frustration.
AI-powered tools in the contact center can address these challenges and help insurers achieve their key value drivers: member enrollment and retention, value-based care, and member experience. AI and automation can be utilized for core call and chat functions, resulting in smarter and more efficient member service.
AI technology can improve both the agent and member experience by meeting the following expectations:
- Consistency and connectedness: Members desire interactions that are consistent and connected with their previous engagements, creating a seamless experience throughout their healthcare journey.
- Personalization: Tailoring the member experience at every step of the healthcare journey is crucial to meet individual needs and preferences.
- Convenience: Members expect convenience, which includes the ability to communicate with their health plan anytime and anywhere.
To deliver what members expect, healthcare insurers must rethink the member experience. Contact center agents play a vital role in building member relationships, serving as the “front door” for most interactions with the health plan. Automation can assist agents by handling simple inquiries, such as prescription requests, through AI-powered voice and digital bots. Natural language processing (NLP) and machine learning enable accurate and intuitive member interactions through voice commands.
AI can also support agents in high-value conversations by providing real-time recommendations and guidance. Agents can rely on AI-powered recommendations to handle complex queries, access up-to-date information, educate members on coverage and cost of care, and provide empathetic support. These recommendations reduce the time and effort required to search for information, enabling agents to focus on delivering a flawless member experience.
Furthermore, AI can provide insights for proactive actions, allowing insurers to take a proactive approach to the member journey. By leveraging intent detection and real-time recommendations, AI can suggest next-best actions and trigger proactive notifications to assist members in scheduling appointments, resolving administrative issues, and improving health outcomes and service.
To reimagine the healthcare member experience, healthcare insurers can utilize Talkdesk Payer Smart Service, an end-to-end solution that delivers connected and convenient experiences by empowering staff and applying intelligent automation to the member journey. This solution enables insurers to provide customized, seamless experiences that differentiate them in the highly competitive market.
In conclusion, AI technology offers significant opportunities for healthcare insurers to enhance the member experience, improve agent performance, and gain a competitive advantage. By leveraging AI-powered tools and platforms, insurers can elevate the member journey, provide tailored and convenient experiences, and meet the rising demands of health insurance members.
To learn more about how AI can improve member experience in healthcare, you can request a free Talkdesk demo to see how their solutions can help improve the member experience.
